HTN | Weekly Health Tech Reads | 3/10
This week's newsletter sponsored by: Ambience HealthcareAmbience Healthcare’s AI operating system has been deployed at UCSF, Memorial Hermann Health System, John Muir Health, The Oncology Institute, and Eventus WholeHealth. By partnering with Ambience, health systems reduce documentation time by an average of 78%, improve coding integrity, and achieve at least a 5x ROI. Their suite of AI applications includes:
If you're interested in sponsoring the newsletter, let us know here.
News
|
While I wish Cigna had included numbers on the Y-axis, it's still a pretty striking chart to look at. Cigna noted that new pharmaceutical products entering the market in 2023 had a median annual price tag of $300,000, a 35% increase over 2022. Cigna views this as a huge opportunity to help manage an affordability crisis that has come along with all this pharmacological innovation. GLP-1s were called out as just one example of the wave that is coming, with the slide also noting the coming wave of gene and cell therapies.
GLP-1s
GLP-1s in particular featured heavily during the session, with Cigna noting they're seeing it as the top challenge their clients are facing. Cigna is launching a new program called Encircle Rx, a "cardiodiabesity value-based care solution." As part of this program, Cigna is providing employers a financial guarantee for GLP-1s in the form of a trend guarantee. Cigna says this allows employers "peace of mind" that they're able to offer GLP-1s for obesity in a manner that the employer can afford. Cigna has partnered with Omada Health as part of this offering to drive lifestyle change, with Omada publishing a retrospective analysis this week finding improved outcomes when coupling GLP-1s with behavior change.
Behavioral health
Cigna announced on Thursday ahead that it is launching a new outpatient behavioral health provider group, Evernorth Behavioral Health Group. During the investor session, Cigna noted it doesn't need to employ providers across the care continuum, but we will see it continue to focus on three high growth segments: behavioral, home based care, and virtual care. The Behavioral Health Group has launched in a few markets and intends to expand nationwide in 2025, guaranteeing it can match patients to a provider who meets their preferences within 72 hours.
Relevant Links:
- Fierce Healthcare: Evernorth expands GLP-1 program, unveils new Behavioral Health Care Group
- Forbes: Cigna's Evernorth to launch behavioral health practice group
- Cigna's 2024 Investor Day presentation
News
CMS revisits Elevance's 2024 Star ratings, giving Elevance a $190 million revenue bump in 2025
Summary: Elevance filed an 8-K on Monday, sharing that CMS agreed to increase Elevance's 2025 Star rating for four plans, meaning that Elevance will have 49% of membership in enrolled in 4-Star plans. Elevance noted that this will increase its 2025 revenue by $190 million. This $190 million happens to be the same amount Elevance was suing CMS for, as covered well in Bloomberg back in January. Elevance leadership noted during an investor presentation at TD Cowen this week that CMS's decision shift was because they agreed with Elevance's argument that the single secret shopper call that dropped those four plans from 4-Star to 3.5-Star should not have counted against Elevance, therefore adjusting those plans back to 4-Star.
My Reaction:
- This was good news for Elevance, which saw a substantial decline in its Stars performance. Based on the comments at TD Cowen, it seems like CMS agreed with at least one of Elevance's two arguments it made in the lawsuit. The one it agreed with was about the TTY line and a call that didn't actually connect to Elevance. It's not clear to me what CMS thought of the other argument that Elevance made, which was that CMS didn't correctly apply the methodology for Tukey outlier deletion. That second question seems like it would have much broader implications for other plans.
- It's also worth noting that SCAN Health Plan filed a similar lawsuit against CMS, seeking $250 million in additional payments because of an issue with a single secret shopper call that went over a time limit. I'd imagine CMS is looking at that issue as well, and it'll be interesting to see what happens with that appeal. It's hard for me to imagine that CMS would look at those issues and agree to bump up the Star rating for Elevance while not doing so for SCAN - it seems like a relatively trivial distinction between the two cases with a massive impact on revenue for the two organizations. Either way, I'd assume other MA plans are taking note of this revision and spending considerable energy examining various Star ratings where they narrowly missed a cut point to see if there is a similar opportunity to appeal to CMS.
Chartis on Medicare Advantage headwinds and market trends
The folks at Chartis released a stellar report on Medicare Advantage enrollment trends that includes some really helpful graphics. The report digs into various trends shaping the future of the MA market, including enrollment, Special Needs Plan growth, plan options and preference, market dynamics & quality, and more.
One chart that caught our eye is the one above highlighting the rapid YoY growth seen in the SNP market.
Assessing retailers performance in primary care following key acquisitions
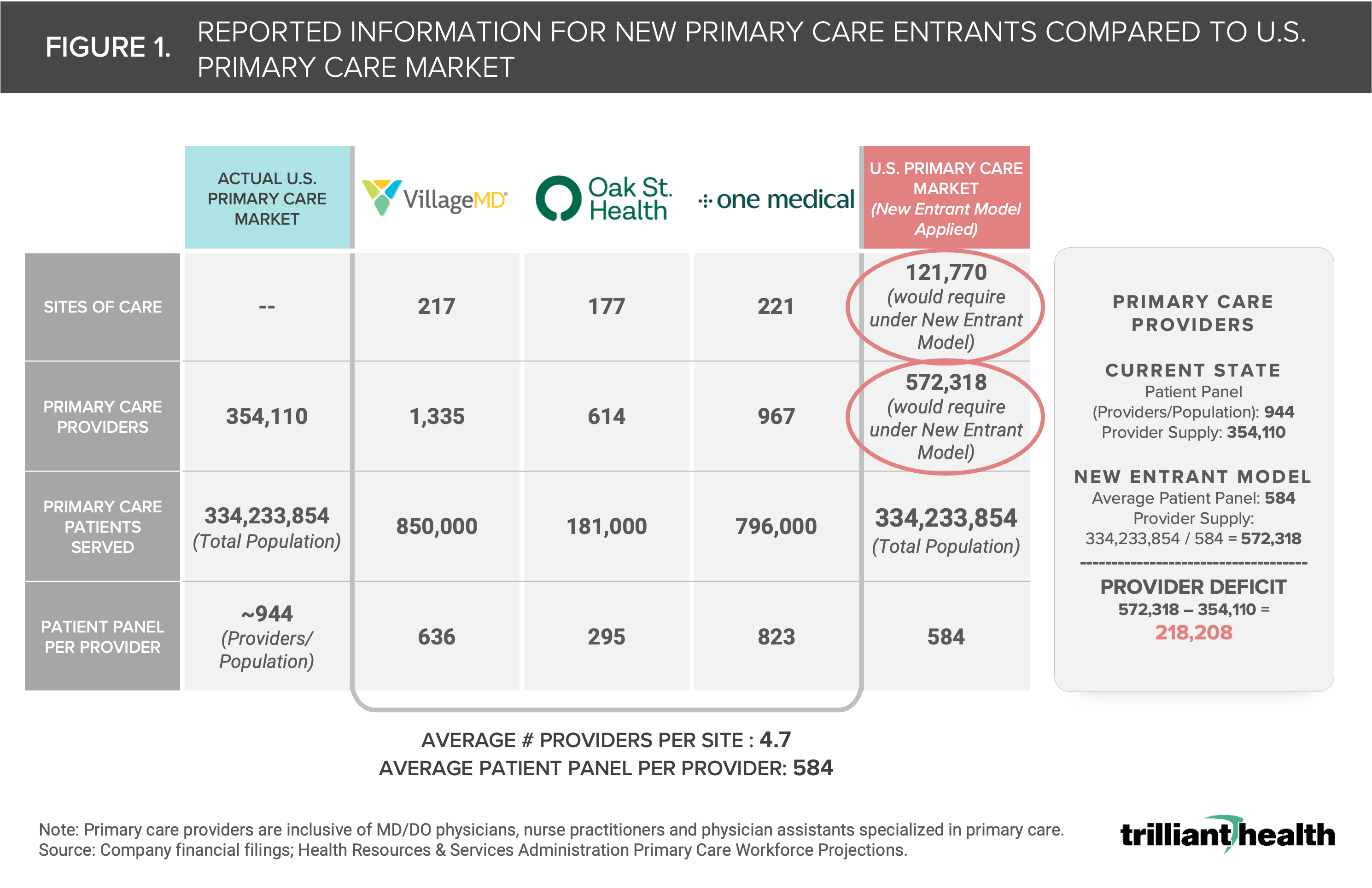 |
Trilliant published an analysis of CVS and Walgreens entrance into the primary care space, focused on the progress by each with their recent acquisitions of VBC providers. The report asks some good questions about the implications of these models, and the chart above highlights some interesting data on the primary care market. Although I always struggle to square the type of data in the left most column describing the overall US primary care market with the idea that we have a primary care shortage. For instance, if you assume a PCP sees patients for 32 hours a week for 48 weeks a year, that would mean that a PCP has 1.5 hours per year for every single patient. Keep in mind that 100 million people in the US also don't have a PCP. If you adjusted the math based on that, it'd imply people with PCPs have 2.3 hours a year with their PCP. What gives?
Aledade’s whistleblower lawsuit provides insight into MSO operations
A two-year old whistleblower lawsuit against Aledade was surfaced by KFF this week after the case was unsealed a few weeks ago. If you’re looking for insight into the types of support that MSO models provide clinicians, the complaint makes for a really good read, irrespective of whether you think Aledade overbilled CMS here or not. The slide above from Exhibit A in the complaint highlights an example of how Aledade was helping PCPs understand how they could make an additional $150k+ by reminding patients with hypertension not to drink alcohol over the holidays. If nothing else, the slide highlights how much grey space there is in the topic of coding.
The Change Healthcare ransomware attack outage continues, although we now have more clarity into when Change expects the outage to be resolved - the payments platform will be back up March 15th, and medical claims will be the week of March 18th. More organizations shared responses to the crisis this week, HHS and CMS. HHS issued a statement on Tuesday, noting that CMS will tell Medicare Advantage plans to remove or relax prior auths and utilization management requirements, among other things. CMS issued two statements, one on Wednesday and one on Saturday. It is considering advance payments for Medicare Part A and Part B, and noted that Medicaid providers are the most impacted and urged Medicaid MCOs to advance payments. Aledade announced it is advancing payments to its partnered provider groups, accelerating $100 million in shared savings to those practices. In terms of the attack itself, it appears that UHG paid a $22 million ransom payment for the data to an affiliate of the hacker. But rather than return the data, the affiliate took that payment and ran off with it, apparently faking a seizure by the FBI in the process. This is meaningful because the hacker apparently still has a copy of all the data and didn't receive their payment. You can't make this stuff up. Meanwhile, it still feels like we're just beginning to feel the ripple effects of all this - UHG has already been hit with six class action lawsuits in the past few weeks.
CardioOne, a physician enablement supporting independent cardiologists in adopting VBC, was acquired by WindRose, a private equity firm. As part of the transaction WindRose will commit up to $100 million in funding to support growth.
Link
A group of senators led by Elizabeth Warren continued their push to rein in MA insurer profitability, sending a letter to HHS and CMS on Monday urging them to ensure that those funds go to providers and patients instead.
Link
Humana and Strive Health, a kidney care provider, are partnering to launch an expanded VBC initiative that will provide members in Indiana, Illinois, Kentucky, Michigan, and North Carolina with access to Strive's kidney care program.
Link
Late last week, Bicycle Health clinicians filed to unionize, citing a shift in company culture over the last few years that has left them feeling increasingly overworked and underpaid. The news release cited growing concerns with leadership decisions and the impact it might have on patient care. Will be worth watching if we see clinicians at other telehealth companies follow suit.
Link
Memora Health, a care enablement platform, announced a partnership with Intermountain Health to help expand expand access to cancer care for patients across Intermountain's health system. The multi-year partnership will start with cancer care and aims to expand to other care workflows.
Link
Kinsa Health, an infectious disease prediction platform based on its smart thermometers, announced its acquisition by Healthy Together, a SaaS company that focuses on disease surveillance, behavioral health management, and benefit enrollment for public health agencies.
Link
Rubicon Founders, a healthcare investment firm helmed by Adam Boehler, raised $1.18 billion for Rubicon Fund II, which is more than double its previous Fund I that closed on nearly $500 million in 2022.
Link / Slack (h/t Rik Renard)
Overjet, an AI platform for dental care, raised $53 million in Series C financing, bringing the company's valuation to $550 million. The company's FDA-approved platform helps dentists detect and quantify oral diseases.
Link
Healthee, an employee healthcare benefits navigation platform, secured $32 million in Series A funding.
Link
Tava Health, an employee mental health company, raised $20 million in Series B funding to enhance product development, expand its provider network and employer & insurer partnerships.
Link / Slack (h/t Rik Renard)
Limbic, a mental health AI startup, raised $14 million in fresh capital to expand access to the company's platform to US-based providers. The company currently serves 260,000 patients across the UK's NHS system.
Link
BrainCheck, a cognitive health assessment startup, secured $15 million in Series B funding. The company has developed a suite of cognitive assessment tools focused on neurodegenerative diseases that it sells to both private practice and health system providers.
Link
Tiny Health, a pediatric at-home gut microbiome company, raised $8.5 million in Series A funding. Since its inception, the company has expanded its suite of products to include adults, children (ages 3-17), and vaginal health to test microbiome health across multiple stages of life.
Link
Chamber Cardio, a tech-enabled cardiology platform, raised $8 million in Seed funding to develop technology, expand its cardiology network, and increase headcount. The company's platform, which includes back office infrastructure tools, VBC contracting support, and care teams, aims to help cardiologists and payors in the shift to value-based care.
Link / Slack (h/t Michael Ceballos)
Bone Health, a company developing a non-invasive wearable for bone health, has raised $5 million. The startup's wearable device aims to help postmenopausal women protect against bone density decline associated with menopause and aging.
Link
2024 Health Equity Trends to Watch by Emily Zhen
This was an interesting lens into how the team at Zeal Capital Partners thinks about its investment thesis in the health equity space and a few emerging trends to watch. The team highlights four major health equity categories - including access & affordability of care, women's health, mental health & wellness, and social determinants of health - and digs into the market dynamics driving interest in these categories.
How LLMs can Improve Care Quality in Behavioral Health, Expand Access, and Accelerate the Shift to Value-Based Care by Arpan Parikh, Amit Parikh, and Luis Voloch
A good perspective on how LLMs will impact the behavioral health space. In particular, how LLMs will enable continuous care delivery, tracking outcome-based metrics to drive to VBC, and the creation of a most robust feedback loop for physicians.
Thinking of selling into the employer? You probably shouldn't by Christina Farr and Peter Hames
As we find ourselves in a world where employee benefit managers are completely overwhelmed by point solution offerings, Farr and Hames make the argument that new startups should not consider targeting the self-funded employer market (with a few exceptions). It's a nice perspective on how the employer market has evolved in recent years, why many point solutions don't address a broad enough need today, offers up some tactical advice for those still looking to push into the market.
Digital health has engagement wrong by Kate Wolin
This article builds on the employer article by Farr and Hames above, focusing on how Omada Health did it right in the employer market.
Chief of Staff at Practice Better, a healthcare practice management software. Link
Lead Product Manager, Platforms at Hims & Hers, a D2C telehealth provider. Link
Vice President, Payer Sales at Elektra Health, a menopause care platform. Link
Senior Associate, Customer Success at Pearl Health, a primary care enablement startup. Link
VP of Brand at Spring Health, a mental healthcare provider. Link
Contact us to feature roles in our newsletter.
Welcome to Health Tech Nerds
Health Tech Nerds is one of the most trusted resources in healthcare, helping our members learn, network, build, and grow to maximize our collective impact on the healthcare system.
This week's newsletter sponsored by: Sidebar Being a senior leader in healthcare can be lonely. Growing your career in this space requires making a lot of tradeoffs and placing bets on what you believe will have the most impact, then doubling or tripling down on that. As a result, it can be challenging to find time to grow a network of supportive peers. Sidebar is here to help change that. Their vetting process and matching engine pair you with a small group of supportive peers to lean on for...
This week's newsletter sponsored by: Elation Health Elation Health, whose primary care EHR and billing solution supports companies including Crossover Health and Firefly Health, is committed to supporting and advancing the interests of primary care organizations. Recently, Elation was among the coalition of companies advocating for G2211, Medicare’s new billing code that ensures PCPs are adequately compensated for their investment in longitudinal care for patients. Elation’s commitment to...
This week's newsletter sponsored by: Medallion As care delivery organizations onboard new providers, many organizations must write off new provider revenue for over 60 days due to lengthy enrollment processes. Given providers average nearly $2,000 in revenue per day, that delay can equate to a loss of $120,000 per provider. With Medallion, this doesn’t have to be reality. In their on-demand webinar, credentialing experts from Medallion will share practical strategies for achieving “day one...